Pre-certification Is Associated With Which Type of Utilization Review?
Utilization direction (UM) is a complex process that works to meliorate healthcare quality, reduce costs, and improve the overall health of the population. This guide explains how it works, who information technology helps, and why it'southward important.
In this article, y'all'll learn virtually the utilization management types of reviews, the procedure flow, and how to implement a UM program.
What Is Utilization Management in Healthcare?
Utilization management (UM) is a process that evaluates the efficiency, appropriateness, and medical necessity of the treatments, services, procedures, and facilities provided to patients on a case-past-case basis. This process is run by — or on behalf of — purchasers of medical services (i.e., insurance providers) rather than by doctors. Hospitals, medical staff, insurers, and patients are all affected by UM.
Medical services evaluated (by and large tracked by per 1000 patients per year) by utilization management tin can include the following:
- Inpatient admissions
- Inpatient days
- Skilled Nursing Facility (SNF) admissions
- SNF inpatient days
- Habitation health visits
- ER visits
- Outpatient visits
Other metrics (usually tracked by number of patients per month or per year) can include primary care physicians visits, specialty referrals, high-toll imaging (MRI, PET, etc.), and toll per visit.
Types of Utilization Direction
UM has iii principal types of reviews: prospective, concurrent, and retrospective. This structure is comparable to the Donabedian model of healthcare quality, adult in the late 20th century past Avedis Donabedian. Each kind of review tin impact the process differently.
- Prospective Review: Performed before or at the onset of treatment, on a instance-by-case ground, this review is designed to eliminate unneeded services. The chosen treatment should be considered contingent, and may be changed later.
- Concurrent Review: This type of review occurs during the course of treatment and tracks a patient's progress and resource consumption; which may cause in-process care procedures to stop.
- Retrospective Review: Conducted after treatment is washed, the review assess the appropriateness and efficacy of the handling in order to provide data for future patients.
Let's take a closer look at each type of review.
Looking for a ameliorate way to manage your resources? Look no farther.
Resources Management by Smartsheet empowers your people to more effectively manage teams across projects, runway time accurately, and forecast with confidence then you tin make better, more informed decisions with a clear view of every project.
Watch the demo
Prospective Review
A prospective review is an analysis of a patient'due south case and their proposed treatment. Its main purpose is to eliminate unneeded, ineffective, or duplicate treatments. A prospective review is used during routine referrals and urgent referrals, only not for ER admissions. The review can occur before or afterward access to a facility, but always earlier treatment begins. In some cases, a dr.'s orders may be overridden, which can cause resentment in the medical staff and patients.
Prospective reviews may also be known as precertification, preadmission certification, admission certification, prior authorization preservice review, or preprocedure review.
Concurrent Review
A concurrent review occurs while handling is in progress and usually starts within 24-72 hours of admission to a hospital. The master focuses of the review are to track utilization of resource and the patient'due south progress, and to reduce denials of coverage later on the treatment is complete. The following are included in the review:
- Care Coordination: Syncing the delivery of a patient'south health care when it comes from multiple providers or specialists.
- Discharge Planning: Determining what needs or milestones need to exist met for a patient to go out the infirmary.
- Care Transition: When a patient moves from ane level of care to another (for case, from ICU to standard care).
During a concurrent review, a service or treatment that's already underway may be stopped, or reviewers may expect for alternatives to ongoing inpatient care or try to begin the belch planning process sooner than the doctor would prefer. These actions may cause conflict between the insurer, the treating md, and the patient.
A concurrent review can also be referred to as a continued stay review or an admission review.
Retrospective Review
A retrospective review is mostly performed subsequently treatment is complete. Its purpose is to appraise the appropriateness, effectiveness, and timing of treatments, likewise as the setting in which they were delivered.
The goal of a retrospective review is to see what treatments work best, so that those can exist prescribed to like patients in the future. It allows reviewers to find bug and successes, and send that data back to caregivers. Yous can besides use this information in pedagogy and during contract negotiations between insurers and hospitals.
If proven treatments are not used, and a claim is denied, the fiscal brunt falls on the caregiver. The process also looks to ensure that reimbursements are accurate, or if a claim should be denied. The review can also be redone if a denial is challenged or to respond to grievances.
A retrospective review tin can also be used at a fundamental juncture of treatment rather than at the end, and the outcome may exist that the patient's treatment reverts back to a previous point. This change happens if the patient has non responded or the diagnosis changes, or if a unlike set of UM criteria comes into play (for example, if the patient's insurance coverage changes).
Why Utilization Management Is Important
Utilization direction began in the 1970s, but became prevalent in the 1980s, as healthcare costs started to rise more significantly than they had in by decades. Insurers and employers were looking for ways to control costs — and ane of the key goals of UM is to keep costs down.
Utilization management looks at the effectiveness of treatments for each patient, both while they are occurring and after they are over. This analysis contributes to the second and third goals of UM, which are improving patient care and increasing the overall health of the population.
Reviewing treatments also contributes to the final goal of utilization management, which is to reduce denials. By using data gathered in a retrospective review, yous can evaluate the effectiveness of treatments. When caregivers prescribe these treatments, insurers are more likely to approve them.
Below are a few other reasons that utilization direction is of import for patients, healthcare providers, and insurance companies:
- In the U.South., health insurance is mainly provided by employers. Increases in healthcare costs impact the profitability and competitiveness of the companies that provide these benefits. The private sector pays for the healthcare of most people under 65 (whether employer or individuals); effective treatments aid ill or injured people get back to being productive, and also relieve money.
- Companies that self-insure assume the financial take a chance of health costs of their employees and dependants. Utilization management tin help forestall 1 person'southward wellness problems from negatively impacting the resources available for other people.
- The costs associated with running a utilization direction program are small compared to the savings it can attain.
- The effectiveness of new and experimental treatments are evaluated and fabricated more available if they are amend or cheaper than existing ones.
- Unnecessary or harmful treatments can exist discovered and stopped.
- The average age of the population is rising, and and so is the need for effective treatment.
The lift pitch for utilization direction could be something like this: "Ensuring that patients receive constructive care at the appropriate time, for the appropriate elapsing of time, delivered at a reasonable cost."
Benefits of Utilization Management
A well-run utilization management program has benefits for all parties involved: patients, healthcare providers, and insurers. The pros for each are as follows:
- Patients: Get lower costs, more than effective treatments, and fewer claim denials.
- Healthcare Providers: Get fewer merits denials, lower costs, more constructive treatments, better data, and better resources deployment.
- Insurers: Get lower costs, ameliorate data, and the evaluation of the effectiveness of new treatments and protocols.
How Utilization Management Tin can Reduce Denials
In utilization management, treatment is evaluated and canonical either proactively (during prospective review) or while in progress (during concurrent review), creating fewer reasons to deny claims.
For case, later a main care md informs a patient that their diagnosis requires surgery (as well as referral to a surgeon), a patient contacts her employer's insurance provider. The insurance provider contacts the surgeon to discuss the following options:
- In discussing inpatient versus outpatient surgery, they see that inpatient procedures have fewer complications, so they opt for that.
- They determine that pre-surgical tests tin exist performed on an outpatient basis.
- Based on those conclusions, they settle on the anticipated post-surgery recovery time and scheduled release date.
Having these conversations in advance means the treatment is less likely to be denied.
How Utilization Direction Can Improve Intendance
In a fee-for-service healthcare model, patients will receive unnecessary and inefficient handling. During the retrospective process of utilization direction, examine the results of treatments and compare them to other treatments. Adjacent, evaluate the data collected during this process and apply the findings to time to come patients in like situations.
Here is another example of how utilization direction improves care: A hospital admits a heart attack patient later on they have been stabilized in the ER. The hospital contacts the patient's insurance provider and they discuss the options for treatment and the optimal length of stay. The insurance provider checks in for progress reports regularly. The doctor says that the original treatment plan is not getting the expected results, so they change to a different treatment that has shown promise in similar patients.
Since the insurance company and doctor worked together to evaluate progress, they were able to discover a course of treatment that could yield better results.
How Utilization Direction Tin Help Contain Costs
As doctors attempt new treatments, each are evaluated for efficacy compared to existing options. Treatments that get results will be covered in the future; those that don't will not be covered going frontwards. The costs associated with running a UM program are pocket-sized compared with the savings that one can achieve.
In improver, the following actions by insurance providers tin can also contribute to the goal of reducing costs:
- Incentives for doctors to prescribe less-costly treatments
- Education and feedback for doctors about constructive care standards and practices
- Gatekeeping to manage patient referrals abroad from expensive services and specialists
- Patient instruction
- Pattern benefits to reward patients and healthcare providers that opt for less expensive treatments
- Contracts with providers that have proven records of cost containment
Doctors believe utilization management should recognize that the treating physician is the key role in the healthcare arrangement. Withal, insurers believe that they, equally the payer, should accept the biggest say. Physician gatekeeping is a term that describes the procedure of an insurer having a major role in choosing when patients could be referred to specialists or provided treatments. In their 2002 paper "Utilization Management: Issues, Furnishings, and Future Prospects," Thomas One thousand. Wickizer and Daniel Lessler wrote, "Physicians have been outspoken critics of utilization management because it has express their clinical autonomy and has contributed to an intolerable administrative burden."
Challenges in Utilization Management
Like whatever procedure, utilization direction isn't perfect. There are issues that tin can create resistance and acrimony among both patients and healthcare professionals, including the following:
- Costs can autumn on patients if post-treatment reviews effect in a denial of benefits.
- Patients may have to bear costs if they don't follow the treatment guidelines of the insurer.
- Patients may sue when coverage is denied, or if an experimental treatment is not permitted.
- Physicians don't ever have the insurer's medical necessity guidelines as their outset consideration when delivering care.
- Concurrent and prospective reviews may overturn wishes of main care physicians.
- The number of reviews are rising, every bit are denials of coverage.
- The process steps required by insurers can be perceived as red record or unnecessary by healthcare workers.
- Physicians may not well-receive the results of retrospective reviews.
- Even with UM in place, the toll of care is nevertheless high, so it may be seen as ineffective.
- There is not-response or non-payment from an insurer (sometimes called de facto deprival).
- Some tests may reduce uncertainty about the patient'southward diagnosis, but not add any data that helps determine if a handling is effective or not. Doctors may see these tests as important, merely insurers might not have the same view.
- The number of insurance providers and the coverage available may cause costs to fluctuate.
- At that place may be a deviation between the all-time practice and almost toll-constructive treatment, which can create a conflict between doctors and insurance companies.
- The procedure tin can exist burdensome on medical staff, taking them away from fourth dimension that could be better spent with patients.
- Review criteria are often subconscious from doctors and patients, then they may non know why coverage is denied.
- UM may not have as large an consequence as was once idea. In the same 2002 paper, Wickizer and Lessler found that "evaluations of UM accept generated mixed findings, with some studies showing reductions in utilization and costs and others showing little consequence."
Reducing coverage denials is one of the key goals of utilization management, but they will not be completely obliterated. There are a myriad of reasons why insurers deny coverage, including the following:
- Contract exclusions, including services that aren't covered or having services performed at facilities that aren't in an insurer's network.
- Prescribed treatments that are unproven or investigational. (However, treatments are constantly under evaluation, so something denied today may be covered in the futurity.)
- Lack of medical necessity of a handling.
- Technical errors in the documentation, such every bit missing or incomplete information.
Utilization Management Procedure Flow
The UM procedure is complex. Requirements will vary by location, partners, and focus of the medical organization. Information technology's impossible to map a process flow that will apply generally, merely you tin start past following the steps in the prospective, concurrent, and retrospective review.
Steps in Utilization Direction
In this section, you'll learn the basic steps that occur in the prospective, concurrent, and retrospective reviews. Not all steps will happen for all patients (for example, an emergency room comprisal for a eye attack volition most probable not have whatsoever prospective review steps), and you may need to repeat some of these steps if y'all appeal a declined treatment.
Prospective Review
- Verify the patient'southward coverage and eligibility of the proposed treatment.
- Collect the patient's clinical information to determine the level of care needed and if the proposed treatment is medically necessary.
- Approve the handling if criteria are met; deny it if not.
- If denied, the doc tin can entreatment.
Concurrent Review
- Continue to collect patient'due south progress, prognosis, cost, and resource usage.
- Insurer reviews data.
- Corroborate to continue or asking to change treatment.
- If a modify is requested, the medico can appeal.
Retrospective Review
- Insurer reviews a patient'south records.
- Based on the results, the insurer may update their criteria for covered treatments.
- In some cases, coverage will be denied at this point.
- If denied, the physician or patient tin appeal.
Implementing a Utilization Direction Program
It takes a lot of time and effort for a healthcare provider to implement a UM program. You lot tin can develop a plan in-house, only at that place are many resources and help available from vendors such equally URAC and National Commission for Quality Assurance (NCQA), as well as useful templates and well-known frameworks, similar McKesson InterQual criteria or MCG.
The following questions will help guide the implementation of a UM program to ensure it meets goals and operates properly:
- How volition the utilization direction programme limit unneeded utilization and incorporate costs?
- What are the potential consequences (both positive and negative) of bringing outside parties into the patient care controlling process?
- Will electric current processes hold utilization direction organizations and purchasers accountable for their actions, or volition you require new forms of oversight?
- What are the responsibilities of healthcare providers and patients?
- What are the responsibilities and authority of case managers and intendance managers on the UM commission?
- How volition you educate patients and staff most the value of UM?
UM programs will need to meet all applicative country and federal insurance guidelines and requirements (e.g., California Regional Healthcare Cost & Quality Atlas, ERISA, Medicare Access and CHIP Reauthorization Act, HIPAA), besides as health plan and payer requirements, including third-party payers (similar the Inpatient Prospective Payment System). You may also need to consider specialty medical society guidelines.
Any hospital that receives reimbursement from Centers for Medicare and Medicaid Services (CMS) is required to implement a programme that provides for review of services furnished by the hospital and its medical staff.
A utilization management program can be run on a trial basis, merely because it may require changes to processes, record keeping methods, and the cosmos of new roles, it may not brand sense to do so.
A UM also needs to be comprehensive. In addition to primary care, pharmacy, advanced care, emergency services, behavioral health, psychiatry and substance abuse, and surgery, you lot'll need to include whatsoever other relevant specialties. Run utilization management daily, on all cases, and document all key steps in social club to provide the best data.
Documentation volition demand basic information like vital signs, diagnoses, and proposed treatment plan. However, more than in-depth data is necessary, such every bit whatever lower-level care alternatives (like outpatient care) that were suggested and why they were not appropriate.
UM Components and Techniques
Utilization management is a complex procedure that has many moving parts. Go on the post-obit in mind:
- Ensure the privacy and confidentiality of patient medical data.
- Internal quality comeback processes and audits will require clinical data, and so you'll demand to prepare up data sharing.
- Treatment decisions volition need to be reviewed and communicated in a timely manner, so delegate tasks and create a responsibility matrix that you lot can manage.
- Justify the medical necessity of admissions, extended stays, and professional services.
- Create a feedback process to evaluate the effectiveness of clinical criteria likewise as satisfaction with the process.
- When an insurer denies treatment, having a review board to process and collaborate with patients will expedite responses (i.e., whether to appeal or have and observe some other treatment).
- When decisions are appealed, a plan should be in place that will allow information to be gathered to support the entreatment.
- ICD-ten is a list of codes used to allocate symptoms and diseases; considering it is used internationally, using it every bit role of UM volition help with communication.
- Incorporate Merit-Based Incentive Payments Organization (MIPS) and Culling Payment Models (APM) into your programme.
- Proactively work to ensure that clinical documentation supports proposed courses of treatment.
- Processes need to be evidence-based, and then they volition require information gathering and verification tools.
- Exist prepared for external audits.
- Ensure that payers and insurers share data in a timely manner.
- Incorporate tools to identify high-risk patients and their affect on the process.
- Pedagogy is crucial for effective utilization management, then fix up programs for patients and staff.
- Include administrative requests for clinical instance reviews.
- Team-based care works well with UM. Primary care physicians should lead teams that work to their highest level, communicate with patients earlier, during, and subsequently in-person office visits, have systems in place to identify gaps in intendance, preventive needs, and clinical pathways, work to support process improvement, and look for system-level trends.
High Cost Example Management
High toll cases — those in which a small number of patients or beneficiaries generate a large portion of covered medical expenses — tin cause headaches for insurers. Information technology'southward estimated that 1 to vii pct of patients tin account for xxx-60 pct of costs. Utilization management case managers focus mainly on reducing costs over other key goals.
While the same steps are used every bit other cases (assessing needs and circumstances, and so planning, arranging, and coordinating the handling), these cases will get extra scrutiny in an attempt to find cheaper treatment options. Often, this pace happens without the patient's consent. However, there is mostly no penalisation if a patient is not willing to comply.
Insurers may opt to cover handling options that they don't usually embrace if it volition cost less than treatments that they ordinarily contract.
High toll case direction can too exist referred to as catastrophic instance direction, large case management, medical case direction, or individual benefits management.
Pharmaceuticals in Utilization Management
There are some aspects of utilization management that are specific to prescribing drugs and tracking their effects. For case, many drugs require prior authorisation before they can be dispensed. This authorization step allows the insurer to verify if at that place are lower-cost or generic options available, and as well reduces the chance of addiction and abuse. Quantity limits also prevent waste matter and reduce the potential for abuse and addiction. Patients can also ask for exceptions and medicines, only these must be approved past the insurer before they volition be covered. Insurers can also track patient adherence to a handling plan past refill rates.
Utilization Management versus Utilization Review
The two terms are occasionally used equally synonyms. Utilization review (UR) is a procedure in which patient records are reviewed for accuracy and completion of handling, later the handling is complete. UR, a separate activity, tin exist a function of UM (specifically during retrospective review), and can bulldoze changes to the UM process.
Utilization Management versus Case Management
Professionals tin can't always agree on the definition of case management, simply according to the Case Management Body of Noesis, it'due south "...a professional and collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to encounter an individual'southward health needs."
Case management promotes patient health, service quality, and cost-effective outcomes.
URAC Standards for Utilization Direction
URAC (which originally stood for Utilization Review Accreditation Committee, but at present has no official meaning) is a not-profit organization that runs accreditation programs for many areas of healthcare (they also provide teaching programs). Ane of their areas of accreditation is utilization management.
URAC works with UM programs to help them ameliorate and meet URAC standards in social club to become and stay accredited. You lot can download a high-level list of URAC'southward standards from their website. Among the of import parts of these standards include the recommended construction of an organisation involved in UM, qualifications needed for fundamental roles, how to manage information, and how to stay in compliance with regulations.
NCQA Utilization Management Standards
NCQA (National Committee for Quality Assurance) is a non-profit that as well operates healthcare-related certification and accreditation programs, including utilization management. Their UM offerings include a framework on which to build a program that aligns with land requirements.
You can read nearly the benefits and the accreditation procedure on their website.
Utilization Management Plan Template
Because UM is such an involved and intertwined gear up of processes and procedures, a simple template would non be helpful. However, the Medicare and Medicaid Atmospheric condition of Participation Tenent Healthcare website contains all-encompassing templates that will give you an thought of the corporeality of work required to ready a UM program.
People and Entities Involved in Utilization Direction
In add-on to the nurses, doctors, hospitals (from small town clinics to well-known facilities like the Mayo Clinic), their staff (including program managers, medical directors, and referral coordinators), private insurance companies (eastward.g., Aetna and Allstate), at that place are a number of other entities that are of import to UM.
- Medicare: A government-run insurance program for people 65 and older.
- Medicaid: A government-run insurance program for low income people.
- Prefered Provider Organization (PPOs): An example of managed intendance. They are health insurance companies that contract with healthcare providers for reduced rates. Blue Cross/Bluish Shield is the best-known example of a PPO.
- Wellness Maintenance System (HMOs): Another type of managed intendance that provides both insurance and healthcare, or works with closely-affiliated entities for healthcare. Kaiser Permanente is a well-known HMO. HMOs are sometimes chosen integrated delivery systems, and they drove the growth of UM in the 1980s. HMOs mostly have higher quality and lower costs than PPOs.
- URAC: An organization that accredits utilization management programs and provides education as well.
- National Association of Insurance Commissioners (NAIC): An entity that sets standards and defines regulations for the insurance industry, including how to implement UM.
- American Hospital Association (AHA): A professional association that is one of the drivers behind UM, and acts as a clearinghouse for national healthcare data for their members.
- Iowa Infirmary Clan (IHA): A regional version of the AHA.
- American Physical Therapy Clan (APTA): An entity that provides data and guidance about UM to its members.
- National Academy of Medicine (NAM): Formerly known as IOM (Institute of Medicine), NAM is affiliated with the National Academy of Science. The organization provides data and communication about health and health policy. It ran an informational board called the Committee on Utilization Direction by Third Parties, which helped ameliorate the effectiveness of UM.
- Recovery Audit Contractors: These people review claims for Medicare and Medicaid to observe and correct errors, improper reimbursement, incorrect coding of services, non-covered services, and duplicate services. They are partly reimbursed based on the improper payments they identify.
- Centers for Medicare and Medicaid Services (CMS): A federal bureau that is involved with the assistants of those programs, plus Fleck (Children'due south Health Insurance Program), the federal health insurance market, and HIPAA (Health Insurance Portability and Accountability Act) program. CMS provides data on healthcare quality and costs to the public.
- Peer Review Organizations (PROs): Groups of local doctors mandated past the 1982 Tax Equity and Fiscal Responsibility Human action that wait at the quality and cost of services to ensure they see Medicare requirements for quality and cost.
- Independent Practice Association (IPA): An association of independent physicians that contracts with care delivery organizations to provide services to managed care organizations like HMOs and PPOs.
- Managed Care Resources: A nurse-owned organization that works with managed care organizations.
- Envolve Healthcare: A individual company that provides services to insurance companies and medical service providers to help them manage their UM programs
- UM Reviewers: People who help resolve conflicts that come up upward when case decisions are disputed or challenged.
- Utilization Direction Nurses: Nurses who work for insurers or hospitals, and are involved in deciding the type of treatment patients receive.
- Clinical Documentation Improvement (CDI) Specialists: People who examine documentation used to communicate with insurers to await for whatsoever red flags or enhancement opportunities.
- Physician Advisors: People who review cases for which the proposed treatment may non be approved, and make recommendations to meliorate the chances of approving. They are sometimes tasked with running the overall UM program.
- Independent Review Organizations (IROs): Organizations that tin can exist tasked with looking at denied claims and supporting or overturning the denials.
Future Considerations in Utilization Management
In some ways, UM already looks to the future. During retrospective reviews, the procedure examines the effectiveness of new and experimental treatments. If they are found to be more effective or cheaper than established ones, they'll exist moved into a preferred position. Trends that may affect utilization management include the following:
- Equally costs continue to ascent, UM may focus more on price containment and assessing the value of treatments than other goals. This act could have negative impacts on patients and doctors.
- Advancements in technology — not only in medical devices and pharmaceuticals, but besides in electronic medical records — will crave the UM process to continually conform, not just in terms of how data is reviewed, but besides in determining what is reviewed.
- The manner medical services are delivered as the population ages may drive change in UM.
- Changes to organizational relationships and concern methods at both hospitals/clinics and insurance providers may strength changes in UM procedures.
- AI and big data may remove the demand for human input on many cases.
Improve Utilization Management Efforts with Smartsheet
A cardinal role of utilization direction is collecting data and reviewing information technology to improve processes and care for patients going frontwards. That'due south why information technology's essential to have a tool that can serve as a primal repository and rails the review process in all stages of treatment.
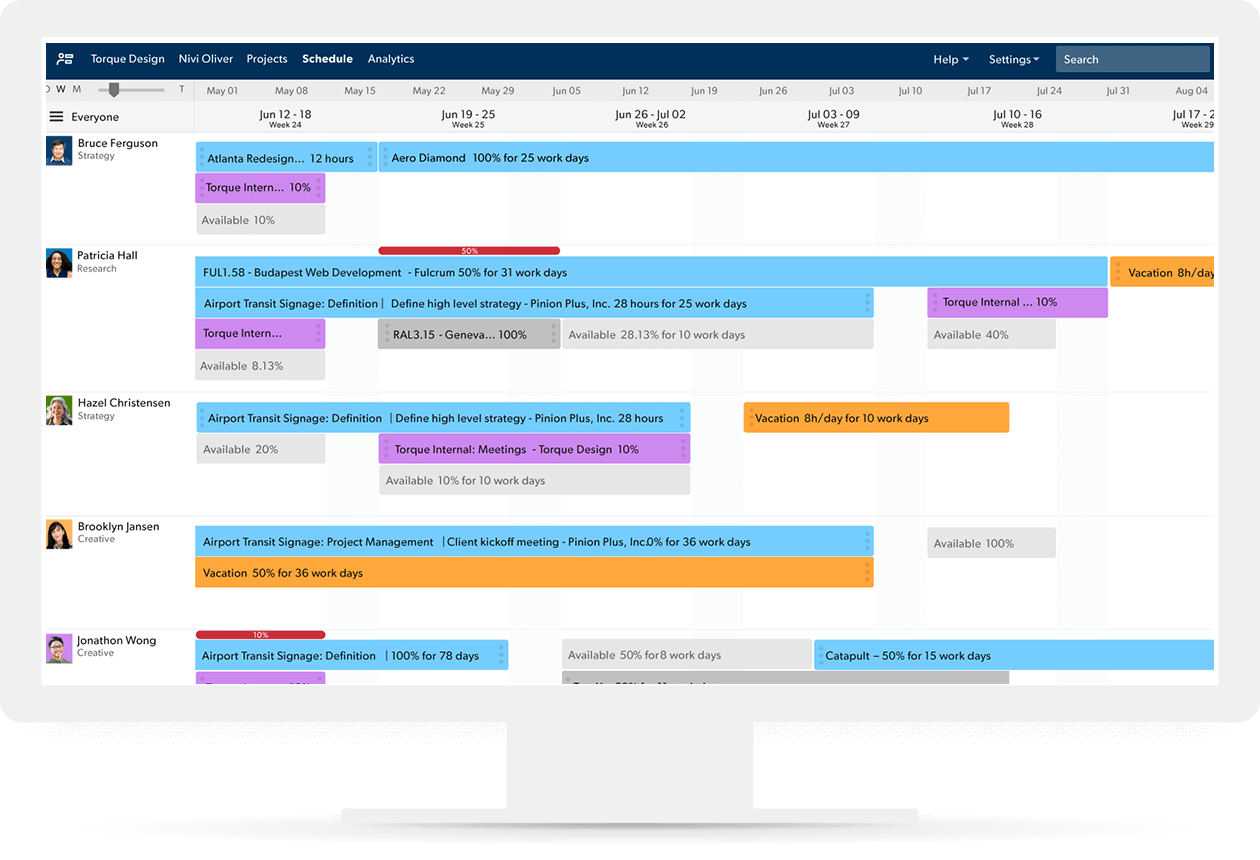
Resource Management past Smartsheet is a powerful resources direction software designed for stronger teams and more than successful projects. With Resource Management, you can more easily build the best team for a projection, keep project schedules and budgets on track, and confidently forecast business concern needs.
Leverage the portfolio-level planning and resource direction capabilities to find and schedule the right resources, view how work is progressing, forecast upcoming hiring needs, and get a complete flick of all moving parts of a project so you lot can see who's available and brand changes as the project moves forrard.
If you lot're looking for a powerful and effective mode to manage your resources, see Resource Direction by Smartsheet in activity.
Watch a gratis demo
Source: https://www.smartsheet.com/content/utilization-management
0 Response to "Pre-certification Is Associated With Which Type of Utilization Review?"
Post a Comment